“The vaccine paradox: We are in a golden age of prevention for older adults, but uptake of existing vaccines among adults is low.” Will the public accept new vaccines?”
Older people in developed countries are more protected than ever from infectious diseases thanks to vaccines against influenza, pneumococcus, and varicella-zoster (shingles). And more good news is on the horizon: the majority of vaccines in the research pipeline target diseases that most severely affect adults.
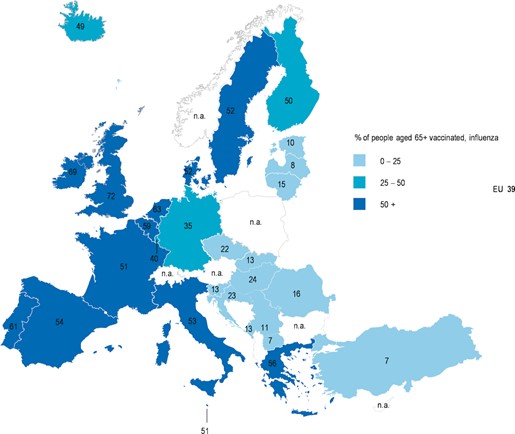
European countries are particularly committed to protecting older people from the potentially devastating effects of influenza. In 2009, health ministers set a target of influenza vaccination for at least 75% of people aged 65 and over. And he made a new commitment for governments to ramp up adult vaccination campaigns in the second half of 2022.
So we’re combining scientific progress with political initiatives, and it’s all very encouraging.That’s the problem Actual intake There are currently insufficient vaccines available for older people in some countries. very low Even other people. In fact, since the target was set in 2009, few countries have achieved 75%. The Netherlands and the UK met their targets a few years ago and have remained close to this level ever since. Portugal, Ireland, Spain and Malta have made significant progress since the coronavirus pandemic.
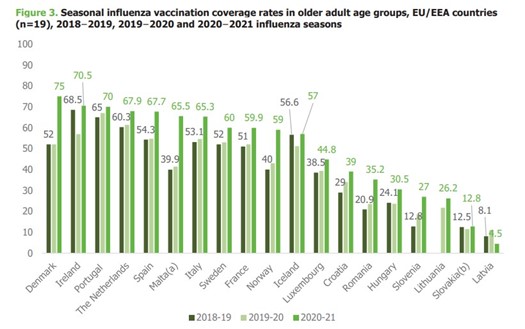
However, of the countries currently reporting to ECDC, only one had an influenza uptake rate of 75% in recently published data. Denmark.
‘Dissonance’ between scientific progress and vaccine rollout
discrepancy between potential Regarding protection and actual vaccination rates, today’s vaccine Webinar on the future of vaccination in Europe. Professor David Salisbury, a Chatham House Fellow, said while new vaccines were coming out, people should take some time to think about the uptake of existing adult vaccines.
“This is a golden age for adult vaccination. We’ve never been more excited about this age group,” he said. “But we have a paradoxical situation: we are making decisions about what could be recommended if it is cost-effective, without focusing on how to get the vaccine to the people who will benefit from it.” We’ve seen all the investments in biotechnology that have led to certain new vaccines.”
Pediatric vaccine uptake has generally been good in Europe, as vaccinations are started according to age and are integrated into pediatric health programs. Vaccines for adults vary by age, are seasonal, and, unlike infant immunizations, are not integrated into the health care system.
Professor Salisbury said influenza vaccination rates were a good indicator of how well the adult immunization program was progressing. He suggested that influenza prevalence among people over 65 is weak and that rolling out many new vaccines to the same population will not work, adding: “If we can’t effectively vaccinate the population, how on earth are we going to do the rest?” Is that so?” he said. ?’
Data collection and use
Countries that do well with influenza vaccination are also likely to do fairly well with pneumococcal vaccination and, in some cases, varicella-zoster vaccination. And these countries tend to have one thing in common: they collect vaccination data and use it to improve vaccination rates.
“There are two things that make a difference and they are intertwined. The first is data and the second is management. You can’t have one without the other,” Professor Salisbury said. I did. “In fact, if you don’t have both, don’t be surprised if your performance is poor.”
Data must be timely, accurate, and individualized to enable decision makers to identify regions and providers where uptake is off target. It is too late to analyze influenza vaccine uptake data at the end of the influenza season.

For example, Denmark invested in a national vaccination registry almost a decade ago and is now reaping the benefits.in a recent interview today’s vaccineDr. Palle Valentaner-Brans, from Denmark’s Statens Serum Institute (SSI), outlined how this could allow authorities to run customized campaigns or send reminders to book a vaccine. .
At the heart of this system is a unique personal identification number known as a CPR. “We have a lot of registries linked to cardiopulmonary resuscitation data. This is an epidemiologist’s dream,” said Dr. Palle Valentine Bruns. “By linking data, we will be able to conduct advanced research on vaccines and vaccination behavior.”
What are we delaying?
Given the success of Denmark, the UK and the Netherlands, it seems natural to wonder why other countries haven’t copied this data-driven approach. Professor Salisbury points out that it’s not a question of large amounts of money or access to complex data management tools.
“Most immunization program registrations are simple databases that can be run on a mobile phone,” he said. “We need a unique identifier, data about who provides care to the individual, and a way to link that with information about vaccination, whether it takes place in a GP clinic, pharmacy or other location. is.”
As we enter a golden age of vaccine technology, now is the time to use data to increase influenza vaccine uptake. The investment in this effort will pay off for individuals and health systems by preparing for the introduction of other vaccines that can not only prevent influenza but also protect older and vulnerable adults.
read more:
Related article
Bridging the gap: A data-driven vision for life course immunizationNovember 10, 2023
How the Danish Vaccination Registry became the basis of Denmark’s vaccination serviceOctober 27, 2023


